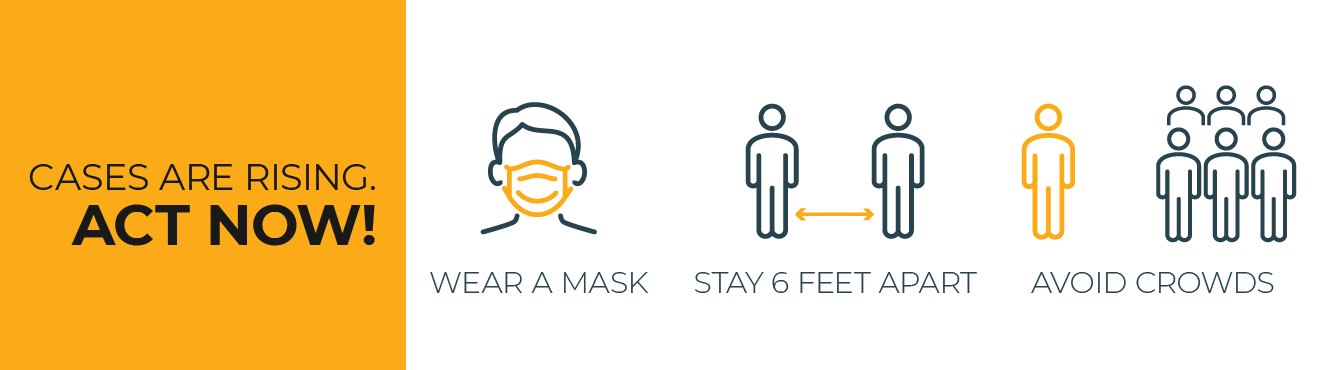
Covid-19 cases, hospitalizations, and deaths across the United States are rising. Take steps to slow the spread of Covid-19.
Coronaviruses (CoV) are a large family of viruses that cause illness ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS-CoV) and Severe Acute Respiratory Syndrome (SARS-CoV).
Coronavirus disease (COVID-19) is a “novel” virus, meaning new strain that was discovered in 2019 and has not been previously identified in humans. Therefore response to this pandemic is constantly changing and evolving with new developments. As cases continue to rise in the U.S., it is important that Laurens County take necessary and logical precautions to reduce the risk of exposure.
The virus is thought to spread mainly from person-to-person who are in close contact with one another (within 6 feet) and through respiratory droplets produced when an infected person coughs or sneezes. These droplets can land in mouths or noses of people nearby or possibly be inhaled into the lungs.
Laurens County officials encourage everyone to take the appropriate steps to protect yourself by wearing a mask when out in public, by washing your hands often with soap and water for at least 20 seconds, use hand sanitizer that contains at least 60% alcohol when soap and water are not available, and by avoiding touching your eyes, nose and mouth with unwashed hands. Put distance between yourself and other people, even if you are both wearing a mask, and avoid close contact with people that are sick. By protecting yourself, you reduce the spread of COVID-19.
Laurens County Emergency Management Press Release on COVID-19
Laurens County Operations Press Release
Laurens County Resolution 2020-19C on Mask Usage
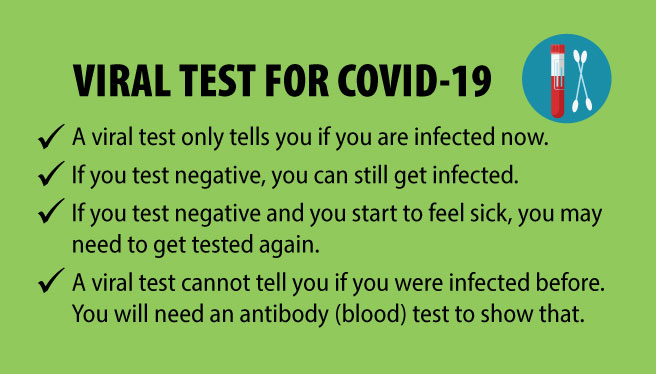
Scheduled Local Testing Sites
No Information on Testing Sites at this time, please check back.
OR check with the Laurens County Emergency Management Team at 864-984-0812
SC DHEC has a drive thru testing site set up at the DSS / DHEC Complex at 93 Human Services Rd, Clinton, SC 29325 Mon – Fri with hours of operations 09:30 – 02:30 each day.
Watch for Symptoms
People with COVID-19 have had a wide range of symptoms reported – ranging from mild symptoms to severe illness. Symptoms may appear 2-14 days after exposure to the virus. Older adults and people who have severe underlying medical conditions like heart or lung disease or diabetes seem to be at higher risk for developing more serious complications. People with these symptoms may have COVID-19:
- Fever or Chills
- Cough
- Shortness of Breath of Difficulty Breathing
- Fatigue
- Muscle or Body Aches
- Headache
- New Loss or Taste or Smell
- Sore Throat
- Congestion or Runny Nose
- Nausea or Vomiting
- Diarrhea
This list does not include all possible symptoms. CDC will continue to update this list as more is learned about about COVID-19.
Covid-19 Vaccines
We understand that some people may be concerned about getting vaccinated now that COVID-19 vaccines are available in the United States. While more COVID-19 vaccines are being developed as quickly as possible, routine processes and procedures remain in place to ensure the safety of any vaccine that is authorized or approved for use. Safety is a top priority, and there are many reasons to get vaccinated.
All COVID-19 vaccines currently available in the United States have been shown to be highly effective at preventing COVID-19. Learn more about the different COVID-19 vaccines.
All COVID-19 vaccines that are in development are being carefully evaluated in clinical trials and will be authorized or approved only if they make it substantially less likely you’ll get COVID-19. Learn more about how federal partners are ensuring COVID-19 vaccines work.
Based on what we know about vaccines for other diseases and early data from clinical trials, experts believe that getting a COVID-19 vaccine may also help keep you from getting seriously ill even if you do get COVID-19.
Getting vaccinated yourself may also protect people around you, particularly people at increased risk for severe illness from COVID-19.
Experts continue to conduct more studies about the effect of COVID-19 vaccination on severity of illness from COVID-19, as well as its ability to keep people from spreading the virus that causes COVID-19.
Clinical trials of all vaccines must first show they are safe and effective before any vaccine can be authorized or approved for use, including COVID-19 vaccines. The known and potential benefits of a COVID-19 vaccine must outweigh the known and potential risks of the vaccine for use under what is known as an Emergency Use Authorization (EUA). Watch a video on what an EUA is.
Getting COVID-19 may offer some natural protection, known as immunity. Current evidence suggests that reinfection with the virus that causes COVID-19 is uncommon in the 90 days after initial infection. However, experts don’t know for sure how long this protection lasts, and the risk of severe illness and death from COVID-19 far outweighs any benefits of natural immunity. COVID-19 vaccination will help protect you by creating an antibody (immune system) response without having to experience sickness.
Wearing masks and social distancing help reduce your chance of being exposed to the virus or spreading it to others, but these measures are not enough. Vaccines will work with your immune system so it will be ready to fight the virus if you are exposed.
The U.S. Food and Drug Administration (FDA) has granted Emergency Use Authorizations (EUA) for two COVID-19 vaccines which have been shown to be safe and effective as determined by data from the manufacturers and findings from large clinical trials. These data demonstrate that the known and potential benefits of this vaccine outweigh the known and potential harms of becoming infected with the coronavirus disease 2019 (COVID 19). Visit the CDC’s Page on Vaccine Safety.
Visit the CDC’s Page on Frequently Asked Questions about the Covid-19 Vaccination.
Vaccine doses purchased with U.S. taxpayer dollars will be given to the American people at no cost. However, vaccination providers will be able to charge an administration fee for giving the shot to someone. Vaccine providers can get this fee reimbursed by the patient’s public or private insurance company or, for uninsured patients, by the Health Resources and Services Administration’s Provider Relief Fund.
Because the U.S. supply of COVID-19 vaccine is expected to be limited at first, CDC is providing recommendations to federal, state, and local governments about who should be vaccinated first. CDC’s recommendations are based on those from the Advisory Committee on Immunization Practices (ACIP), an independent panel of medical and public health experts.
The recommendations were made with these goals in mind:
- Decrease death and serious disease as much as possible.
- Preserve functioning of society.
- Reduce the extra burden COVID-19 is having on people already facing disparities.
CDC recommends that initial supplies of COVID-19 vaccine be allocated to healthcare personnel and long-term care facility residents. This is referred to as Phase 1a. Phases may overlap. CDC made this recommendation on December 3, 2020.
CDC recommends that in Phase 1b and Phase 1c, which may overlap, vaccination should be offered to people in the following groups. CDC made this recommendation on December 22, 2020.
Phase 1b
- Frontline essential workers such as fire fighters, police officers, corrections officers, food and agricultural workers, United States Postal Service workers, manufacturing workers, grocery store workers, public transit workers, and those who work in the educational sector (teachers, support staff, and daycare workers.)
- People aged 75 years and older because they are at high risk of hospitalization, illness, and death from COVID-19. People aged 75 years and older who are also residents of long-term care facilities should be offered vaccination in Phase 1a.
Phase 1c
- People aged 65—74 years because they are at high risk of hospitalization, illness, and death from COVID-19. People aged 65—74 years who are also residents of long-term care facilities should be offered vaccination in Phase 1a.
- People aged 16—64 years with underlying medical conditions which increase the risk of serious, life-threatening complications from COVID-19.
- Other essential workers, such as people who work in transportation and logistics, food service, housing construction and finance, information technology, communications, energy, law, media, public safety, and public health.
The goal is for everyone to be able to easily get a COVID-19 vaccination as soon as large enough quantities of vaccine are available. As vaccine supply increases but remains limited, ACIP will expand the groups recommended for vaccination.
Other Resources
- Vaccine Considerations for People who are Pregnant or Breastfeeding
- How CDC Is Making COVID-19 Vaccine Recommendations
- Role of the Advisory Committee on Immunization Practices in CDC’s Vaccine Recommendations
- Covid 19 Vaccine FAQ Info-Graphic from SCDHEC
New Covid-19 Variants
Information about the characteristics of these variants is rapidly emerging. Scientists are working to learn more about how easily they might spread, whether they could cause more severe illness, and whether currently authorized vaccines will protect people against them. At this time, there is no evidence that these variants cause more severe illness or increased risk of death.
Viruses constantly change through mutation, and new variants of a virus are expected to occur over time. Sometimes new variants emerge and disappear. Other times, new variants emerge and persist. Multiple variants of the virus that causes COVID-19 have been documented in the United States and globally during this pandemic.
Multiple COVID-19 variants are circulating globally. In the United Kingdom (UK), a new variant has emerged with an unusually large number of mutations. This variant seems to spread more easily and quickly than other variants. Currently, there is no evidence that it causes more severe illness or increased risk of death. This variant was first detected in September 2020 and is now highly prevalent in London and southeast England. It has since been detected in numerous countries around the world, including the United States and Canada.
In South Africa, another variant has emerged independently of the variant detected in the UK. This variant, originally detected in early October, shares some mutations with the variant detected in the UK. There have been cases caused by this variant outside of South Africa. This variant seems to spread more easily and quickly than other variants. Currently, there is no evidence that it causes more severe illness or increased risk of death.
Another variant recently emerged in Nigeria. CDC also is monitoring this strain but, at this time, there is no evidence to indicate this variant is causing more severe illness or increased spread of COVID-19 in Nigeria.
Scientists are working to learn more about these variants, and more studies are needed to understand:
- How widely these new variants have spread
- How the new variants differ
- How the disease cause by these new variants differs from the disease caused by other variants that are currently circulating
Public health officials are studying these variants quickly to learn more to control their spread. They want to understand whether the variants:
- Spread more easily from person to person
- Cause milder or more severe disease in people
- Are detected by currently available viral tests
- Respond to medicines currently being used to treat people for COVID-19
- Change the effectiveness of COVID-19 vaccines. There is no evidence that this is occurring, and most experts believe this is unlikely to occur because of the nature of the immune response to the virus.
How to Protect Yourself and Others
Know how it spreads
- There is currently no vaccine to prevent coronavirus disease 2019 (Covid-19)
- The best way to prevent illness is to avoid being exposed to this virus.
- The virus is thought to spread mainly from person to person.
- Between people who are in close contact with one another (within about 6 feet).
- Through respiratory droplets produced when an infected person coughs, sneezes or talks.
- These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs.
- Some recent studies have suggested that Covid-19 may be spread by people who are not showing symptoms.
Everyone should
- Wash your hands often with soap and water for at least 20 seconds especially after you have been in a public place, or after blowing your nose, coughing or sneezing.
- It’s especially important to wash:
- Before eating or preparing food
- Before touching your face
- After using the restroom
- After leaving a public place
- After blowing your nose, coughing or sneezing
- After handling your mask
- After changing a diaper
- After caring for someone who is sick
- After touching animals or pets
- If soap and water are not available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
- Avoid touching your eyes, nose and mouth with unwashed hands.
Avoid close contact
- Inside your home: Avoid close contact with people who are sick.
- If possible, maintain 6 feet between the person who is sick and other household members.
- Outside your home: Put 6 feet of distance between yourself and people who don’t live in your household.
- Remember that some people without symptoms may be able to spread virus
- Stay at least 6 feet from other people
- Keeping distance from others is especially important for people who are at higher risk of getting very sick
Cover your mouth and nose with a mask when around others
- You could spread Covid-19 to others even if you do not feel sick.
- The mask is meant to protect other people in case you are infected.
- Everyone should wear a mask in public settings and when around people who don’t live in your household, especially when other social distancing measures are difficult to maintain.
- Masks should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated or otherwise unable to remove the mask without assistance.
- Do NOT use a mask meant for healthcare workers. Currently, surgical masks and N95 respirators are critical supplies that should be reserved for healthcare workers and other first responders.
- Continue to keep about 6 feet between yourself and others. The mask is not a substitute for social distancing.
Cover coughs and sneezes
- Always cover your mouth and nose with a tissue when you cough or sneeze or use the inside of your elbow and do not spit.
- Throw used tissues in the trash.
- Immediately wash your hands with soap and water for at least 20 seconds. If soap and water are not readily available, clean your hands with a hand sanitizer that contains at least 60% alcohol.
Clean and disinfect
- Clean AND disinfect frequently touched surfaces daily. This includes tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks.
- If surfaces are dirty, clean them. Use detergent or soap and water prior to disinfection.
- Then, use a household disinfectant. Most common EPA-registered household disinfectants will work.
Monitor your health daily
- Be alert for symptoms. Watch for fever, cough, shortness of breath, or other symptoms of COVID-19.
- Especially important if you are running essential errands, going into the office or workplace, and in settings where it may be difficult to keep a physical distance of 6 feet.
- Take your temperature if symptoms develop.
- Don’t take your temperature within 30 minutes of exercising or after taking medications that could lower your temperature, like acetaminophen.
- Follow CDC guidance if symptoms develop.





Call 911 if you have a medical emergency
Notify the Operator that you have or think you may have COVID-19. If possible, put on a facemask before medical help arrives.